Malaria & Neglected Tropical Diseases
Highlighting the commitment from the Kigali declaration and looking at how we can deliver political and financial commitment to eradicate malaria and NTDs and avoid resurgence. This Mediaplanet campaign was distributed with the Guardian newspaper and launched on www.globalcause.co.uk on 16-May 2022
Highlighting the commitment from the Kigali declaration and looking at how we can deliver political and financial commitment to eradicate malaria and NTDs and avoid resurgence.
This Mediaplanet campaign was distributed with the Guardian newspaper and launched on www.globalcause.co.uk on 16-May 2022
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Q2 2022 | A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content
Read more at www.globalcause.co.uk
Malaria & Neglected
Tropical Diseases
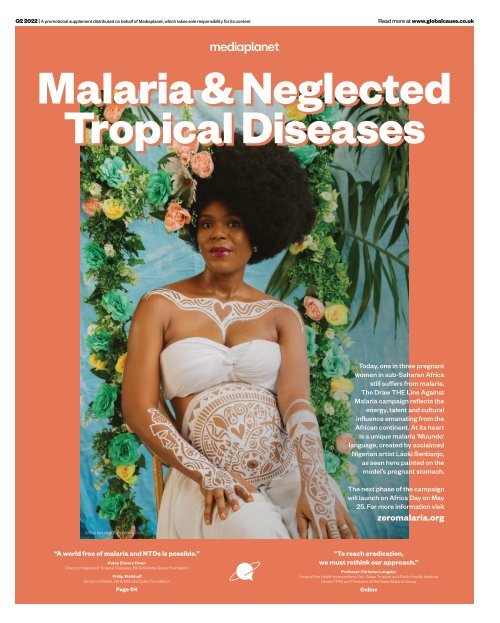
Today, one in three pregnant
women in sub-Saharan Africa
still suffers from malaria.
The Draw THE Line Against
Malaria campaign reflects the
energy, talent and cultural
influence emanating from the
African continent. At its heart
is a unique malaria ‘Muundo’
language, created by acclaimed
Nigerian artist Láolú Senbanjo,
as seen here painted on the
model’s pregnant stomach.
The next phase of the campaign
will launch on Africa Day on May
25. For more information visit
zeromalaria.org
©ZERO MALARIA/ THOMPSON S. EKONG
“A world free of malaria and NTDs is possible.”
Katey Einterz Owen
Director, Neglected Tropical Diseases, Bill & Melinda Gates Foundation
Philip Welkhoff
Director, Malaria, Bill & Melinda Gates Foundation
Page 04
“To reach eradication,
we must rethink our approach.”
Professor Christian Lengeler
Head of the Health Interventions Unit, Swiss Tropical and Public Health Institute
(Swiss TPH) and President of the Swiss Malaria Group
Online
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS
We can end NTDs
but we must show our
commitment now
2022: A pivotal moment
for a more equal world
Incredible progress has been made against neglected tropical diseases (NTDs)
but there is still work to be done. The Kigali Declaration on NTDs, a new political
declaration, provides the opportunity to end NTDs.
NTDs are a group of 20
diseases that affect 1.7
billion people globally; they
can debilitate, disfigure
and kill. These diseases include
elephantiasis, rabies, river blindness
and trachoma. We call these diseases
neglected because they affect the
world’s poorest and they receive less
attention than other diseases.
The effects of NTDs are devastating,
they impair cognitive and physical
development in children. They
lead to school and work absences,
particularly in women and girls
who are often responsible for caring
for their family. They also cost the
economies of endemic countries
billions of dollars and can trap
communities in cycles of poverty.
Recognising the success so far
Over the past decade, incredible
progress has been made against NTDs.
So far, 44 countries have eliminated
at least one NTD and 600 million
people no longer require treatment
for NTDs. Some of these diseases that
have plagued humanity for centuries,
such as leprosy, sleeping sickness and
guinea worm disease are also at an alltime
low. This shows that ending NTDs
is within our power, but there is still
work to be done.
The Kigali Declaration on NTDs
pushes us forward
The Kigali Declaration on NTDs is a
new high-level political declaration
that will launch later in 2022 at the
Kigali Summit on Malaria and NTDs,
alongside the 26th Commonwealth
Heads of Government meeting. The
Kigali Declaration will put country
ownership of NTD programmes,
integration and cross-sectoral
collaboration at the front and centre
to ensure that these programmes are
sustainable in the long term.
The Declaration provides the
opportunity to mobilise the political
will, community commitment,
resources and action needed to end
unnecessary suffering from NTDs.
Signatories of this declaration
pledge to do their part to ensure that
NTDs are eradicated, eliminated or
controlled by 2030.
Commitment to ending NTDs is needed
By working together, adopting peoplecentred
approaches and working
across sectors in an integrated manner,
we can end NTDs and achieve WHO
2030 NTD road map targets. Now
is the moment for leaders, donors,
companies and organisations to
make endorsements behind the
Kigali Declaration and show they are
100% committed to ending NTDs.
These commitments will help relieve
needless suffering, decrease the
health-related drivers of poverty, make
our health systems more resilient and
our world an equitable and safer place.
For more information visit 100percentcommitted.com
WRITTEN BY
Thoko Elphick-Pooley
Executive Director,
Uniting to Combat
Neglected Tropical
Diseases
Ending malaria and NTDs will save lives, advance equity and build resilience.
Over the past two years, no
country has been spared
the impacts of COVID-19, a
deadly infectious disease that
killed millions, infected millions and
devastated communities, economies
and health systems. The same impacts
can be attributed to malaria and
neglected tropical diseases (NTDs)
however, these diseases have been
around for millennia and typically
prey on the world’s poorest in Africa.
Ending preventable and treatable diseases
In 2000, global leaders committed
funding and action to reduce cases
and deaths caused by these diseases.
Thanks to this strong political will
and increased funding, by 2015
malaria deaths were cut by over
half and more than 5 billion NTD
preventive treatments were delivered.
The tremendous progress achieved
through global collaboration and
commitment prompted more
ambition to end these preventable
and treatable diseases by 2030.
In the case of malaria, a turning
point was the launch of the Global
Fund to Fight AIDS, Tuberculosis
and Malaria. Significantly, 20 years
later, the Global Fund, working with
the US President’s Malaria Initiative
and country partners, has saved 44
million lives.
But in the last two years, progress
has slowed and cases and deaths are
on the rise. With challenges of drug
and insecticide resistance, COVID-19
and humanitarian emergencies, the
world is at a precarious juncture in the
fight against malaria.
Better prepared for better results
However, there is hope on the horizon.
Thanks to greater country ownership,
better use of data and targeting of
existing and new tools, a pipeline
of transformative tools and strong
political will. And, if governments,
the private sector, communities and
partners come together later this year
to fulfil the Global Fund’s Seventh
Replenishment goal of at least USD 18
billion, we can turbocharge progress
again toward a malaria-free future.
By mobilising new funding, we can
scale up existing and breakthrough
tools, including new nets and vaccines
and better target interventions to the
local context. We also must invest
more in research and development to
deliver transformative new tools, such
as second-generation vaccines, that
will accelerate our path to malaria
eradication.
Critically, these innovative
approaches will also help countries
strengthen their health systems,
allowing them to better protect citizens
against malaria and NTDs and be
better prepared for future pandemics.
With COVID, we’ve seen what the
world can do when it comes together.
Let’s recommit to saving millions more
lives from malaria and NTDs, invest
in health and deliver a more equitable
world for all.
WRITTEN BY
Dr Corine Karema
Interim CEO, RBM
Partnership to End
Malaria
Read more at
campaign.co.uk
@GlobalcauseUK @MediaplanetUK
Contact information: uk.info@mediaplanet.com or +44 (0) 203 642 0737
Please recycle
Industry Manager: Benedetta Marchesi benedetta.marchesi@mediaplanet.com Campaign Assistant: Mia Huelsbeck Managing Director: Alex Williams Head of Strategic Partnerships: Roz Boldy |
Head of Production: Kirsty Elliott Senior Designer: Thomas Kent Design & Content Assistant: Aimee Rayment | Digital Manager: Harvey O’Donnell Paid Media Strategist: Jonni Asfaha Social & Web Editor:
Henry Phillips Digital Assistant: Carolina Galbraith Duarte | All images supplied by Gettyimages, unless otherwise specified
02 MEDIAPLANET
READ MORE AT GLOBALCAUSE.CO.UK
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS
Image provided by The Carter Center
This is how we finish off Guinea worm
In the past 200 years, humankind has made incredible progress against many threats to health: vaccines, medicines and other innovations
have saved millions of lives from feared killers, from malaria to cancer. But only one human disease – smallpox – has ever been eradicated.
WRITTEN BY
Dr Tedros Adhanom
Ghebreyesus
Director-General, World
Health Organization
WRITTEN BY
Jason Carter
Chair, Board of Trustees,
The Carter Center
Find out more at
cartercenter.org
A
massive campaign has now driven polio to the
brink of eradication, but less noticed by the rest of
the world, we stand on the threshold of consigning
another disease to the history books: Guinea worm.
While Guinea worm is largely unknown to people in highincome
countries, it has afflicted people in Africa, Asia and
the Middle East for millennia.
Last year there were just 15 reported cases of Guinea worm
disease, compared with an estimated 3.5 million in 1986,
when The Carter Center and the World Health Organization
launched the Guinea Worm Eradication Program. Since
then, our two organisations have worked closely with
governments, the US Centers for Disease Control and
Prevention, and partners including the United Arab
Emirates, which hosted the Guinea Worm Summit
in Abu Dhabi in late March.
The official name of Guinea worm is Dracunculus
medinensis, which derives from the Latin for “little dragon,”
and for good reason. People contract the disease by drinking
untreated water that contains tiny fleas that harbour larvae,
which grow in the intestine into worms up to one metre long.
About a year later, they emerge through painful blisters on
the skin. Those infected can’t work or go to school while a
worm is emerging. Extracting a worm from the body can take
a week or longer and is an excruciating process.
There is no vaccine to prevent infection and no medicine
to treat it. But what pharmaceuticals couldn’t do, the
Guinea Worm Eradication Program has accomplished with
humble water filters, a basic larvicide, and the partnership
of millions of people, in some of the world’s poorest
countries, who made simple changes in their behaviour.
Of course, simple doesn’t mean effortless or troublefree.
Progress has been bumpy, complicated by poverty,
the remoteness of affected communities, storms, floods,
droughts, conflict, and, most recently, a pandemic. In 1995,
former US President Jimmy Carter had to negotiate a cease
fire to enable health workers safe passage in the midst of
Sudan’s civil war. Through all this, the communities in
which we work have taken ownership and continued their
unceasing efforts.
Today, Guinea worm disease remains endemic in just five
countries: Angola, Chad, Ethiopia, Mali and South Sudan.
Two other countries – the Democratic Republic of the
Congo and Sudan – are on the path to being certified free of
the disease. Although Cameroon is certified, it is addressing
recent cross-border infections.
At the Summit in the UAE, we joined Ministry of Health
representatives to discuss the Abu Dhabi Declaration on the
Eradication of Guinea Worm Disease.
The declaration reaffirms that the governments of
the endemic countries and we, their partners, will
work urgently for eradication by 2030. It calls for active
leadership nationally and locally, sufficient budget support,
robust implementation of interventions, transparent
communication, rapid provision of safe water everywhere
and safety for health workers.
Preventing the spread of Guinea worm from one
country to another is also critical to accelerate the global
interruption of transmission and requires strengthening
cross-border surveillance and collaboration. Several
countries have made commendable efforts in this direction,
with support from WHO.
We applaud the leaders of the countries who made these
commitments, but they can’t do it alone. Now other global
leaders need to marshal the sustained funding to finish the
job. The last mile of disease eradication is complex, and
momentum can wane as the numbers get close to zero,
especially as other urgent health crises emerge. But if we fall
short of eradication, the disease could return to its former
levels, which would bring needless suffering and economic
challenges to poor communities.
We stand tantalisingly close to a monumental victory for
public health – and for humanity. The eradication of Guinea
worm will be the fulfilment of President Carter’s vision and
the culmination of decades of difficult and often dangerous
work in partnership with some of the poorest, most isolated,
most marginalised people on Earth.
The real heroes in the Guinea worm story are the
thousands of volunteers in more than 23,000 villages who
do the hard work in their own communities. Defeating this
scourge is a triumph of persistence and people, more than
technology and medicine. Village by village, across sub-
Saharan Africa and parts of Asia, citizens have mobilised
and organised to safely treat water sources, distribute
filters, and spread the word on how to change behaviours to
protect themselves and their children.
The victory will be theirs when, sometime before the end
of the decade, 15 cases become zero. To get there, all of us
must do our part to travel the last mile in eradication and
move toward a world free of Guinea worm and the terrible
suffering it brings.
Paid for by
The Carter Center
READ MORE AT GLOBALCAUSE.CO.UK MEDIAPLANET 03
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS
Tackling malaria and
NTDs contributes to more
resilient health systems
People living in fragile settings are the most at risk
of contracting malaria and NTDs yet they are the
least likely to have access to adequate health care.
Building the capacity of local health
facilities and community health
workers to prevent, diagnose and treat
malaria and NTDs in fragile settings
can lead to more resilient health systems and
greater global health security overall.
According to Dr Lali Chania, Tanzania
Country Director of IMA World Health:
“Health systems in fragile settings, if
they exist at all, are beset by external and
internal challenges, including but not
limited to violence, lack of infrastructure
and resources, corruption, access inequities,
weak governance and limited human capital.
Yet fragile settings have a higher disease
burden than other low-income countries.”
Poor public health perpetuates the cycles
of poverty and fragility and vice versa.
As the number of fragile settings increases,
so too does global insecurity and economic
instability. That is why IMA World Health
is committed to health systems
strengthening in fragile settings.
Building on malaria and NTD programming
successes
“The local partnerships, trust and capacities
we have built through our malaria and NTD
programming in fragile settings are key for
any health systems strengthening efforts
to be successful in these complex
environments,” says Chania.
In the Democratic Republic of the Congo
and South Sudan, the organisation has
collaborated with local health facilities
to improve access to malaria prevention,
diagnostic and treatment services for more
than 11.4 million people.
Across Tanzania and Haiti, 28.8 million
people are no longer at risk for lymphatic
filariasis since IMA has strengthened the
capacity of local health systems to sustainably
administer NTD control measures. IMA’s
health partners in these fragile settings are
leveraging these capacities to meet other
critical health care needs.
Dr Chania suggests: “The surveillance
and case-based notification and response
capacities required to eliminate malaria
and NTDs are also what is required to stop
epidemics from becoming pandemics, like
COVID-19. Integrating those capacities into
health systems will not only improve that
system’s resilience to the shocks common
in fragile settings, it will improve global
health security.”
Paid for by IMA World Health
Find out more at
imaworldhealth.org
WRITTEN BY
Dr Lali Chania
Director, IMA
Tanzania Country
Investing in
ending malaria
and NTDs for
a safer world
A world free of malaria and NTDs is
possible. Investing now to end these
diseases will save millions of lives and
protect against future pandemics.
This year, the global community has two
historic opportunities to recommit to
ending malaria and neglected tropical
diseases (NTDs)—by mobilising at least USD
18 billion to replenish the Global Fund to Fight AIDS,
Tuberculosis and Malaria and by supporting the
Kigali Declaration on NTDs to deliver the targets set
in the World Health Organization’s NTD Roadmap
(2021-2030).
Supporting national malaria and NTD programs
Enormous strides have been made against these
diseases since 2000. Global Fund investments helped
scale up lifesaving interventions, contributing
to over 10 million deaths averted from malaria.
The 2012 London Declaration on NTDs, signed by
governments, pharmaceutical companies, endemic
countries, global health organisations, and the Bill &
Melinda Gates Foundation, nearly doubled medicine
donations by the pharmaceutical industry—reaching
over a billion people a year from 2017 to 2019.
Yet these diseases continue to take lives and put
billions of people at risk— and COVID-19 further
hinders progress.
We can end malaria and NTDs and keep us safer
from future health threats. By supporting national
malaria and NTD programs that drive progress
against these diseases, boosting investments, and
better integrating these programs into national
health systems millions of lives can be improved
and saved.
Community-based disease monitoring and tracking
With the goal of ending malaria and NTDs, the Gates
Foundation co-invests and partners with national
programs, pharmaceutical companies, product
development partnerships, research institutes
and global and local NGOs. A primary focus is on
increasing the use of digitised data systems for realtime
disease monitoring to better target delivery of
interventions.
For example, Initiatives like Visualize No More
Malaria and the Lymphatic Filariasis Campaign
Digitization in India are generating valuable insights
at the community level that support decision-makers
to transform healthcare delivery.
Community health workers are at the heart of
national malaria and NTD programs, providing
essential services for millions of people—often in
remote regions. The trust built with the communities
they serve provides a foundation for digitised disease
©Speak Up Africa
monitoring and adaptation of services to emerging
health needs, like COVID-19, showcasing how investments
in malaria and NTDs can help prevent future
pandemics.
Increased financial and political commitments
We are already seeing examples of commitments
and approaches that are helping malaria and NTD
programs to drive lasting progress.
Twenty five sub-Saharan African countries
have launched local Zero Malaria Starts with Me
campaigns and End Malaria Councils to mobilise
country resources and action. The African Union
and Uniting to Combat NTDs recently signed an
agreement to end NTDs by 2030. We are also seeing
critical accountability mechanisms emerge with the
integration of NTDs into national health strategies
and the African Leaders Malaria Alliance scorecard.
To support this stepped-up leadership, global
leaders must join in solidarity and increase funding
to deliver a safer, more equitable world free of malaria
and NTDs.
WRITTEN BY
Katey Einterz Owen
Director, Neglected
Tropical Diseases,
Bill & Melinda Gates
Foundation
WRITTEN BY
Philip Welkhoff
Director, Malaria,
Bill & Melinda Gates
Foundation
©Speak Up Africa
Community health workers are at the
heart of national malaria and NTD
programs, providing essential services
for millions of people.
04 MEDIAPLANET
READ MORE AT GLOBALCAUSE.CO.UK
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS
Institute will shine its light on disease elimination at summit
The forthcoming Kigali Summit provides an opportunity for knowledge to be shared to help combat malaria and neglected tropical diseases (NTDs).
INTERVIEW WITH
Simon Bland
CEO, Global Institute
for Disease Elimination
(GLIDE)
WRITTEN BY
Sheree Hanna
Paid for by
Global Institute for
Disease Elimination
Launched at the end of 2019, the Global Institute
for Disease Elimination (GLIDE), a non-profit
organisation based in Abu Dhabi, is committed to
helping its partners go further and faster towards the
elimination and ultimate eradication of infectious diseases,
with a current focus on malaria, polio, lymphatic filariasis
and onchocerciasis.
The Institute was jointly founded by His Highness Sheikh
Mohamed bin Zayed Al Nahyan, the Crown Prince of Abu
Dhabi, and the Bill and Melinda Gates
Foundation, and builds upon a longstanding
history of investment in global
health.
GLIDE’s CEO, Simon Bland, says: “The
Kigali Summit comes at a time where
some of the world is seemingly emerging
from COVID-19, so understanding its
impacts and lessons will be vitally
important as we look ahead.
“We need more money for health,
but also more health for the money.
We need efficiencies, synergies, effective coordination and
cooperation and synchronicity of services provision across
diseases. We want to help break down barriers and silos.”
Finding the best outcome
Bland says a successful Summit for GLIDE would result
in high-level political commitment from across the
Commonwealth for disease elimination, with increased
commitments to tackling neglected tropical diseases (NTDs),
We need efficiencies, synergies,
effective coordination and
cooperation and synchronicity of
services provision across diseases.
and momentum for a successful Global Fund replenishment
in September.
The Summit will be held alongside the 26th
Commonwealth Heads of Government (CHOGM) meeting in
Rwanda in June.
The rationale behind eliminating or eradicating infectious
diseases means no longer having to invest or survey them,
thereby freeing up money and resources for other priorities.
Bland says: “Calling to end disease is a bold statement of
ambition which can excite, motivate
and attract strong political will for
such an audacious goal. However,
there is a caveat: it is easier to call for
elimination than to deliver it, and the
last mile of elimination is the hardest.”
Innovation is main objective
Innovation is a key objective for the
Institute, which looks to foster and
scale innovation not only for new
tools and technologies, but also for
new strategies for health systems strengthening. GLIDE
is working with partners to convene community, country
and global experts to explore the rationale for programme
integration, keeping in mind that efforts should result in
improved outcomes for all health programmes involved.
The Kigali Summit is an opportunity not only for
galvanising political commitment, but also for stakeholders
from the malaria and NTD communities to identify potential
opportunities for joint advocacy, programming and finance.
Find out more at
glideae.org
Taking a multisectoral
approach in the fight
against malaria
Malaria does not exist in isolation and will require a cross-sector
response through coordination, policy and funding at global and
national level to ensure a malaria-free future for all.
INTERVIEW WITH
Joseph Lewinski
Multisectoral Malaria
Project Lead, Catholic
Relief Services
WRITTEN BY
Meredith Jones
Russell
This cross-sector response
to malaria is called
multisectoral programming.
It uses different sectors to
help bridge funding gaps in malaria
programming, increasing access
and use of malaria services in
communities that are often missed.
Joseph Lewinski, Multisectoral
Malaria Project Lead at Catholic
Relief Services (CRS), explains: “I
don’t think we have seen a country
that has eliminated malaria without a
multisectoral approach.”
Sectors driving the biggest impact
include agriculture, education,
humanitarian response, urban
development, extractive industries,
population movement and defence.
CRS is investing in multisectoral
programming to help ensure these
critical connections are made,
especially in countries with the highest
number of malaria cases.
Image provided by
Catholic Relief Services
“This concept, which has existed
since the first malaria elimination
efforts, proports that by including
other sectors in programming, we can
address common causes that help
spread malaria in endemic countries
and develop malaria ‘smart’ policy to
mitigate their effect,” Lewinski says.
Dual impact approach
Multisectoral approaches have a
positive impact on both malaria
prevalence and on the other sectors
involved.
“By working with the education
sector, you get more consistent access
to children, who are more likely to
be impacted by malaria,” Lewinski
explains. “You can train teachers to
identify signs and symptoms and
strengthen referral system so kids can
get diagnosed and treated quicker.”
“In rice farming agriculture,
increased production can impact
mosquito breeding and, thus, malaria
transmission. A multisectoral
approach can provide dual impact,
in this case, ensuring productive
agriculture production and also in
reducing malaria prevalence. Globally,
malaria stakeholders need to adopt
proactive policy. National malaria
control programmes are needed.
On a community level, farmers and
communities must be considered in
the decision-making process.”
Working towards elimination
In some circumstances, multisectoral
programming can help countries
eliminate malaria completely.
“Multisectoral programs have
historically been used to help reach the
last few cases within countries close
to elimination,” Lewinski explains.
“In the Mekong sub-region, we see that
by working with extractive industries
we can ensure we know where forest
working populations are and find those
last cases.”
But Lewinski emphasises
multisectoral approaches can benefit
all countries with malaria cases.
“This isn’t just an approach for
countries eliminating malaria. By
setting up these systems in high
burden countries, we can ensure this
holistic, integrated response, which
is vital for meeting malaria control
and elimination goal. It just requires
upfront investment, and bringing
together stakeholders who wouldn’t
normally work together, to create
practical and novel solutions.”
Paid for by
Catholic Relief
Services
Scan the QR code
to find out more
READ MORE AT GLOBALCAUSE.CO.UK MEDIAPLANET 05
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS
The health of women
and children is threatened
by a treatable disease
Pregnant women, teenage girls and children remain
disproportionately vulnerable to malaria.
Malaria is one of the world’s
oldest, deadliest diseases,
stealing young futures and
claiming the life of a child
every minute, despite being treatable,
preventable and beatable.
The heavy human cost of malaria
can be measured in the number of
each and every life lost and the many
more that are diminished, with the
latest World Malaria Report revealing
241 million cases and 627,000 deaths
worldwide in 2020 - the highest
number of deaths in nearly a decade.
Malaria deaths are increasing
Tragically, millions of pregnant
women, adolescent girls and young
children remain disproportionately
vulnerable to malaria, with the
disease cited as the third highest
cause of death in teenage girls aged
15-19 in sub-Saharan Africa in 2019.
Despite substantial efforts to
continue malaria services during
COVID-19, disruptions resulted in
an additional 47,000 malaria deaths
in 2020 and, with the impacts of
the pandemic ongoing, so too are
disruptions to healthcare. The
pandemic has also weakened
economies and exacerbated alreadyfragile
health systems which paints an
even darker picture for the health of
women and children going forward.
Limited access to preventable treatment
In 2020, a staggering 11.6 million
pregnant women contracted malaria
across sub-Saharan Africa, and more
than two-thirds of eligible women
across 33 African countries did not
receive the full course of preventive
malaria treatment (IPTp-SP)
recommended by the World Health
Organization.
Malaria in pregnancy has been
associated with maternal anaemia,
exposing the mother to an increased
risk of death before, during and after
childbirth. The dangers are also
substantial for the newborn child,
including low birth weight which
can impact growth and cognitive
development.
Achieving key global malaria targets
One third of the Global Fund to Fight
AIDS, Tuberculosis and Malaria’s
investment goes towards building
inclusive health systems, ensuring
that women and girls have access to
quality health services for malaria
and sexual and reproductive health.
This helps boost progress toward key
global malaria targets and supports
many of the Sustainable Development
Goals including fighting poverty,
improving gender equality and
universal health.
The Global Fund’s seventh
replenishment target this Autumn is
to raise at least USD 18 billion to fight
the three diseases, which would save
20 million lives, cut the malaria death
rate by 64% and build a healthier,
more equitable world, making the
UK’s financial commitment to ending
malaria more critical than ever.
Malaria is a disease that this
generation can end, but only
if we act now.
WRITTEN BY
James Whiting
CEO, Malaria No More UK
Genuine intersectoral
collaboration needed to
achieve better progress
against vector-borne NTDs
WRITTEN BY
Ashok Moloo
Information Officer,
WHO Department of
Control of Neglected
Tropical Diseases
WRITTEN BY
Dr Raman Velayudhan
Head, Veterinary Public
Health, Vector Control
and Environment,
WHO Department of
Control of Neglected
Tropical Diseases
This article was
originally published
on the World Health
Organization’s
website. Scan the
QR code to access
the original article
The world needs to work better and collaborate with
sectors beyond health to implement the Global Vector
Control Response 2017–2030 (GVCR).
The silent spread of vectors over the years means
more countries are now exposed to arboviral
diseases, with human activities facilitating their
survival and propagation.
“It is time that vector control programmes work jointly with
city planners, environmentalists, engineers and sectors that
manage water and sanitation,” says a leading expert during a
WHO-hosted webinar on ‘Reducing the burden and threat of
vector-borne diseases to achieve the NTD road map targets.’
“We face the prospect of seven out of 10 people living in cities
and urban areas globally by 2050.”
Focussing on prevention
“One of the things which is critical as we build out future
cities … we really need to do better in the area of prevention
… reducing the habitats of all mosquito species,” says
Steve Lindsay, panellist and former Professor at Durham
University, United Kingdom.
This implies reducing the breeding sites for Aedes
mosquitoes that transmit vector-borne diseases such as
dengue, chikungunya, yellow fever and Zika. This can be
done by enhancing access to piped water, constructing
houses with built-in screens to block mosquito entry,
clearing waste, improving drainage and keeping the
environment clean.
More than half the world’s population is at risk of
infection from vector-borne diseases.
Challenges to meet targets
While the GVCR is on track for some activities, amounting to
an almost 10% reduction in global mortality over the past five
years, for many other activities targets have not been reached.
A progress report outlining achievements and challenges
will be submitted to the 75th World Health Assembly in
May 2022.
Assessing global risk
More than half the world’s population is at risk of
infection from vector-borne diseases, especially dengue,
leishmaniasis and malaria.
Vectors are responsible for transmitting many neglected
tropical diseases, mostly among the poorest populations
where there is a lack of access to adequate housing, safe
drinking-water and sanitation.
During the past two decades, many vector-borne diseases
have emerged or re-emerged, spreading to new parts of the
world. Dengue alone has increased six-fold since 2000 and
it affects over 130 countries and still there are no effective
drugs, vaccines and sustainable vector control tools, making
it more neglected.
Other factors, such as environmental changes, increased
international travel and trade, changes in agricultural
practices and rapid, unplanned urbanisation have
facilitated the spread of many vectors worldwide.
Current efforts to address the needs for better diagnostics,
vaccines and sustainable innovative vector control
interventions such as the use of Wolbachia, spatial repellents
etc are encouraging new hope in the horizon to address the
void and meet the goals set in the NTD roadmap 2021-2030.
06 MEDIAPLANET
READ MORE AT GLOBALCAUSE.CO.UK
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS
We need to be more adaptable to
control the resurgence of malaria
spatially contextualised information.
This can be delivered via different
innovative systems.
For example, in Equatorial Guinea,
MCD is using a tablet application
(CIMS) to collect and use field-level
malaria control data at the household
and individual levels. Meanwhile, in
other countries, MCD is supporting the
integration of major health information
databases to a common platform.
“Having a more efficient way of
entering, processing and analysing
data is a big benefit in the fight against
malaria,” says Julie Niemczura, Senior
Program Manager at MCD. “Real-time
access to information shortens the
feedback loop so that any deficiencies
can be corrected immediately.”
INTERVIEW WITH
Guillermo García
Senior Program
Manager, Bioko Island
Malaria Elimination
Project, Medical Care
Development
In recent years, malaria cases have been on the rise. The disease
transmission has changed — so the response to it must change
too with a new, adaptive approach based on evidence and data.
Image provided by MCDI
An adaptive approach isn’t
simply beneficial for controlling
malaria. It can also promote
sustainable health systems,
strengthening their ability to
respond rapidly and effectively
to unforeseen challenges.
INTERVIEW WITH
Olivier Tresor Donfack
Technical Coordinator,
Bioko Island Malaria
Elimination Project, Medical
Care Development
Paid for by Medical
Care Development
International
Controlling malaria
is — and has always
been — a mammoth
challenge. Decades
after the first Global
Malaria Eradication
Programme was
launched in 1955, this
life-threatening disease still brings
untold misery and death to many parts
of the world. Indeed, malaria cases are
on the increase. According to figures
from the World Health Organization,
there were 241 million cases in 2020
compared to 227 million in 2019.
There are a number of reasons
for this rise, says Guillermo García,
Senior Program Manager, Bioko Island
Malaria Elimination Project at MCD,
a global public health non-profit
providing interventions across several
health areas. “There are challenges,
for example drug and insecticide
resistance,” he says.
Understanding why there
is a resurgence in malaria
Climate variability may also be partly
responsible for the resurgence, as
warmer temperatures and increased
rainfall make better breeding
conditions for mosquitoes; plus, the
behaviour of mosquitoes is changing.
“In some areas, there is evidence
that insects are biting earlier in the
evening, before people are indoors
or protected by bed nets,” says
Olivier Tresor Donfack, Technical
Coordinator, Bioko Island Malaria
Elimination Project, MCD.
To make matters worse, malaria
control has faced huge funding
constraints — and increased
competition due to the global
pandemic. This has hit resource-poor
communities particularly hard as
they face a disproportionate burden of
illness, death, and declining economic
productivity, welfare and wellbeing.
Benefits of an adaptive
evidence-based approach
To effectively respond to the
resurgence and ultimately achieve
elimination, it’s imperative that
funding for malaria control continues.
“Of course, any tools that are proven
to work should continue to be
deployed,” says García. “But in this
fight, there is often a need for more
innovation and adaptation.” After all,
when traditional methods of malaria
control prove inadequate, new
approaches must be found.
This is why it’s important to adapt
and optimise malaria control strategies
through evidence-based decision
making, based on the use of real-time
Building local capacity with
training and support
Not all solutions have to be hi-tech.
“In some health facilities, wall charts
filled out by hand are a simple way to
track trends,” says Niemczura. “But
how ever health managers receive
the information, it’s crucial that they
know how to use the systems and
interpret the data to affect positive
outcomes.” This requires building
local capacity with robust training
and support, delivered via different
institutional partners.
An adaptive approach isn’t simply
beneficial for controlling malaria. It
can also promote sustainable health
systems, strengthening their ability
to respond rapidly and effectively to
unforeseen challenges and emerging
threats, such as the COVID-19
pandemic. “In Equatorial Guinea, a
team that was fully trained to deliver
clinical trials for malaria was quickly
able to adapt to meet the demands of
COVID-19,” remembers García.
Yet despite the increase in malaria
cases, it’s important to keep things
in perspective. “The resurgence does
not mean that control programmes
are failing,” stresses Donfack. “In
fact, we’re optimistic that trends
will change — if programmes adopt
adaptive control measures based on
evidence and data.”
INTERVIEW WITH
Julie Niemczura
Senior Program
Manager, Medical Care
Development
WRITTEN BY
Tony Greenway
Find out more at
mcd.org
READ MORE AT GLOBALCAUSE.CO.UK MEDIAPLANET 07
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS
Invest in
malaria and
NTDs to fight
future disease
outbreaks
On World Malaria Day, and ahead of the malaria & NTD summit in
Kigali, Rwanda, it is important we recognise the role of strengthening
health systems to prepare for the next global disease outbreak.
©James Roh/Cotopaxi Foundation
WRITTEN BY
Andrea Lucard
Executive Vice
President of Corporate
Affairs, Medicines for
Malaria Venture
WRITTEN BY
Michelle Childs
Head of Policy
Advocacy, Drugs for
Neglected Diseases
initiative
Paid for by Medicines for
Malaria Venutre (MMV)
Before the COVID-19 pandemic, the term
“global health” was often used with
reference to low and middle-income
countries. If the past two years have taught
us anything, it is that we are all “global
health”—North or South, rich or poor, microbes and
particles connect us all.
This World Malaria Day is the perfect time to
recognise that investments in combatting diseases
that often occur amongst the poorest populations
allow countries to build more resilient health
systems. These systems can be deployed in response
to the next global health emergency.
Unlocking innovation
Outbreaks are more likely to occur where health
systems are fragile, and treatment and prevention
tools are scarce. When financial incentives for health
research are low or non-existent, such as in the
context where malaria and neglected tropical diseases
(NTDs) prosper, product development partnerships
(PDPs) are a proven path to unlocking innovation.
The PDP model leverages partners from the public
and private sectors to innovate health tools where a
single entity would be unable or unwilling to take on
the investment.
Since their establishment around 20 years ago, a
small community of 12 PDPs have delivered more
than 65 new health technologies that have protected
and saved the lives of more than 2.4 billion people.
Highlights from two of these PDPs include the
first new single-dose treatment to prevent malaria
relapse in over 60 years, developed in partnership
by Medicines for Malaria Venture (MMV) and GSK;
and the first all-oral treatment for sleeping sickness,
developed by the Drugs for Neglected Diseases
initiative (DNDi), Sanofi and the National Sleeping
Sickness Control Programme in the Democratic
Republic of Congo.
Preparing to combat future outbreaks
From the laboratory to the patient, PDPs have
engaged the populations they serve, helping to
expand local expertise and strengthen healthcare
systems. These capabilities can be called upon to fight
disease outbreaks when new health crises emerge.
In Africa, PDPs have helped strengthen local
capacity to research the world’s most neglected, often
deadly, diseases, such as visceral leishmaniasis and
sleeping sickness. DNDi has supported the training
of laboratory technicians, nurses and physicians
to conduct state-of-the-art clinical research for the
treatment of NTDs. In 2020, these trained resources
were quickly mobilised to launch the ANTICOV clinical
trial – a large trial to find treatments for mild-tomoderate
cases of COVID-19 in low-resource settings.
In addition to supporting local research
capability, PDPs are also working to build on
existing manufacturing capacity for medicines
closer to where they are most needed. With only
around 375 pharmaceutical manufacturers, Africa’s
public sector relies disproportionately on imported
medicines for malaria and NTDs – COVID-19
highlighted this vulnerability.
With funding from Unitaid, MMV is supporting
a Kenyan pharmaceutical manufacturer, Universal
Corporation Ltd, and two Nigerian manufacturers,
Emzor and Swipha, in the development of WHOprequalified
preventive medicines for malaria in
pregnancy. This increased self-sufficiency within the
continent will potentially provide not only adequate
supplies of these life-saving medicines, but also
quality-assured medicines for other diseases.
Like other tropical diseases, malaria thrives where
access to basic health services is limited. Common
symptoms, such as fever, have been shown to mask
indications of other infections, including COVID-19.
This burdens health systems and allows for disease
to spread undetected across borders. Through a
project supported by MMV, Transaid (UK) and
Zambia’s National Malaria Control Programme, local
community members — be they fisherman, farmers,
or primary school teachers — use training systems
established for malaria to inform fellow community
members about COVID-19 related policies, such as
handwashing and social distancing.
PDPs invest where others do not and this is
crucial to strengthening global health security.
The next health emergency is likely just around
the corner. In preparation for this inevitability,
sustained and flexible support to the invaluable
work of PDPs is needed.
Find out more at
mmv.org
08 MEDIAPLANET
READ MORE AT GLOBALCAUSE.CO.UK